Stress Management
Heartmath Transforms Stress to Create Health and Resilience

Heartmath can be the solution!
Accumulated stress is often the underlying cause of illness and makes any illness worse as well as magnifies emotions such as anxiety, anger, depression, lack of sleep, and more.
Heartmath can help you manage the physical and emotional effects of tension, stress, anxiety, and uncertainty. Our response to stress can be managed with the right training and it takes seconds to minutes to balance your nervous system and manage your emotions.
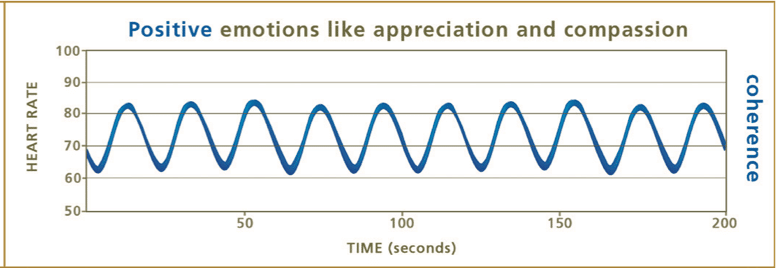
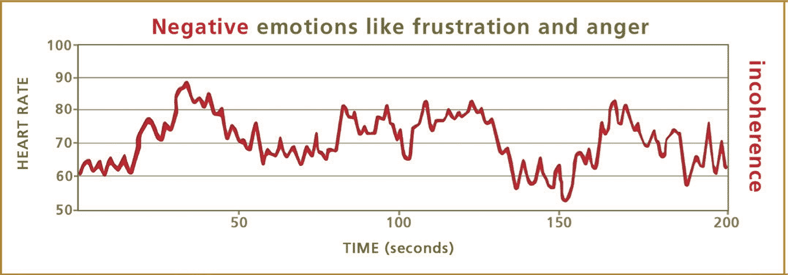
Emotions have a powerful impact on the mind and body. Positive emotions like appreciation, care and kindness feel good and are good for us. They help the systems in our body synchronize and work better.
When we intentionally shift to a positive emotion, the heart rhythms immediately change. This shift in heart rhythms creates a balance of the sympathetic fight or flight nervous system with the parasympathetic rest, digest, rejuvenate, repair and calming nervous system as well as e cascade of neural, hormonal, and biochemical events that benefit the entire body.
The HeartMath Institute has been researching the heart-brain connection for over 25 years and understands how the heart influences our perceptions, emotions, intuition, and health. Their research demonstrates that different patterns of heart activity have different effects on your thoughts and behaviors.
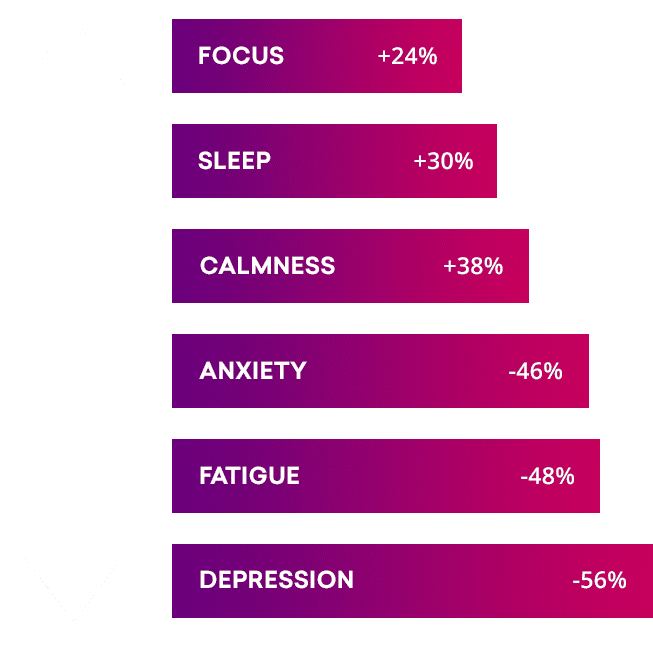
You can achieve these benefits and more!
You can become more resilient, energized, joyful, patient, mentally clear, intuitive and more!
With the right training you can transform stress into success. When we are stressed, the body is out of sync and healing, good decision making, health enhancing neurotransmitters, hormones, and the immune works against us.
Feelings like anger, frustration, anxiety and worry, lead to disorder in the nervous system. Renewing emotions like appreciation, care and kindness create order, which is called coherence. Coherence leads to mental clarity, creativity, and resiliency.
Go from Stress to Success
This simple scientifically validated technique has been used by CEO’s and elite athletes and is available to you.
To get the training you need to go from stress to success contact kathy@vibranceforlife.com or 973 218-1199 x 2.